Roshini Beenukumar, PhD
The human blood-brain barrier (BBB) is a multicellular physiological barrier that controls transport of substances between the blood and the central nervous system. In a study published in Cell Stem Cell, Vatine et al. combined two powerful technologies – iPSC and Organ-Chip technologies – to generate functional and patient-specific human BBB-Chips that recapitulate the functional characteristics of human BBBs including any disease-specific defects.
The blood-brain barrier
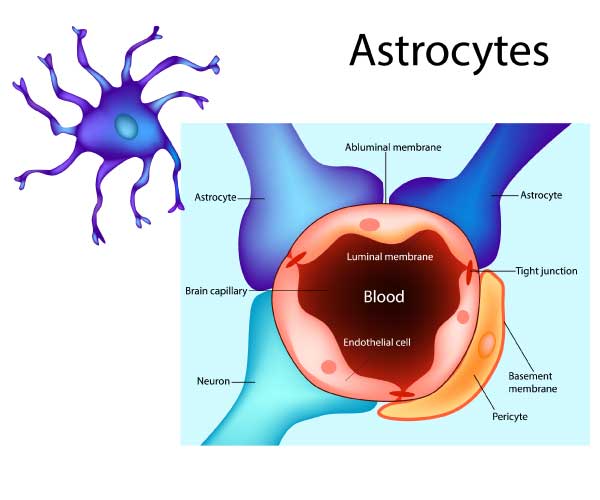
The BBB is a network of blood vessels with unique properties that traverse the central nervous system. It strictly regulates the movement of substances such as molecules, ions, and cells (including drugs) between the blood and the CNS. As with other blood vessels, endothelial cells form the wall of the BBB blood vessels. The unique properties of these brain blood vessels can be largely attributed to this endothelial layer or brain microvascular endothelial cells (BMECs).
Tight junctions between BMECs are responsible for this diffusion barrier, which results in a high transendothelial electrical resistance (TEER). Specialized efflux transporters (to eliminate substrate-drugs from the brain) and influx carriers (to carry essential nutrients into the brain) are found on the BBB endothelium. Additionally, BMECS are induced and maintained by interactions with multiple other cell types such as pericytes, astrocytes, microglia, and neurons.
In vitro cell culture BBB models
Multiple cell culture models of the human BBB have been developed over the years to study BBB biology and drug transport to the brain. Earlier models constituted isolated brain endothelial cells which we later expanded to co-cultures of endothelial cells with other cells of the BBB such as glioma cells, astrocytes, and pericytes. Most of these cell culture BBB models were based on pig, bovine, rat, and mouse cells, as human tissue is usually difficult to obtain. However, immortalized human brain endothelial cells and human stem cell-derived endothelial cells have been developed to circumvent this problem.
Disease models of the BBB have also been developed to study how the BBB is altered in disease states, such as in stroke, Alzheimer’s disease, cancer, and multiple sclerosis. However, BBB models of genetic brain disorders are currently inadequate. Novel models based on human stem cells or iPSCs from patients, like the ones described in this study, have the potential to greatly advance our understanding of BBB biology in these disease states and develop personalized therapies.
A functional, fully human BBB-Chip using iPSC and Organ-Chip technologies
Previous studies have established human iPSCs differentiated into BMEC-like cells, which are structurally and functionally similar to the BBB, including physiologically relevant TEER. However, these established iPSC-derived models of the BBB use 2-dimensional Transwell inserts, which do not fully recapitulate the in vivo microenvironment of the BBB (for e.g., they do not allow direct cell-cell interactions between BMECs and other cells of the brain microvasculature, and lack physiological mechanical forces such as shear stress). The BBB-Chip model developed by Vatine et al. overcame many of these limitations. They used iPSCs to generate a functioning blood-brain barrier inside an Organ-Chip.
Organ-Chip technology uses microfluidic culture devices to mimic the 3D cellular microenvironment. The simplest organ-on-chip systems use a single, continually perfused microfluidic chamber to culture one type of cell. More complex organ-chips such as BBB organ-chips use two or more microchannels connected by porous membranes, lined on opposite sides by different cell types, to recreate interfaces between different tissues.
The BBB-Chip described in the study used human iPSCs on an Organ-Chip platform to functionally recapitulate the interactions between BMECs and human neural cells. The BBB-Chip showed (1) physiologically relevant TEER values, (2) low paracellular permeability, (3) response to inflammatory cues at the organ level, (4) transport of soluble biomarkers, and (5) active efflux pumps. Moreover, the human iPSCs differentiated into BMEC-like cells also formed blood vessel-like structures capable of sustaining blood flow.
A personalized human BBB system for disease modeling and drug screening

Several neurological disorders such as Parkinson's disease, Huntington's disease, and Lou Gehrig's disease) are linked to BBB defects. Interindividual variability may cause variations in patient responses to drugs. Personalized BBB chips, derived from the patient’s iPSCs, have the potential to address this issue. The paper describes two patient-derived disease models – a Huntington BBB-Chip model and a model for Allan-Herndon-Dudley syndrome, a rare congenital neurological disorder characterized by the deficiency of monocarboxylate transporter 8 (MCT8), a specific transporter for thyroid hormone T3. The BBB-Chip models rederived from iPSCs from patients recapitulated the defects observed in these patients – MCT8-deficient BBB-Chips constructed using patient-derived iPSCs showed significantly lower blood-to-brain T3 permeability and the BBB-Chip derived from a Huntington disease patient showed a significant increase in dextran-FITC molecule permeability. These observations suggest that patient-derived iPSC-based BBB-Chips may be used to predict interindividual variability in BBB functions and to deliver personalized therapy.
“The study's findings open a promising pathway for precision medicine. The possibility of using a patient-specific, multicellular model of a blood-brain barrier on a chip represents a new standard for developing predictive, personalized medicine.”, said Dr. Clive Svendsen, Ph.D., Director of the Cedars-Sinai Board of Governors Regenerative Medicine Institute and corresponding author of the study.
Conclusion
The BBB regulates brain homeostasis by acting as a strict gatekeeper. Understanding the biology of the BBB is important to design drugs that can pass this barrier as well as to treat diseases where the BBB functions are altered. Although in vitro cell culture models of the BBB have been around for some time, making them physiologically close to the in vivo BBB has always been a challenge. By combining iPSCs with Organ-Chip technology, this study takes us one- step closer to the ideal in vitro BBB model. The ability to model diseases by using patient-derived cells to create personalized BBB-Chips is another important highlight of the study.
Future Directions
This study and similar other studies using iPSC and Organ-on-Chip technologies provide a new way to understand brain physiology and diseases. Also, further iterations of these BBB models could one day help us to accurately predict which drugs would work best for individual patients, paving the way for personalized medicine for neurological disorders.
"Stay informed with the latest news from PHCbi”
参考文献
1. Vatine, G. D. et al. Human iPSC-Derived Blood-Brain Barrier Chips Enable Disease Modeling and Personalized Medicine Applications. Cell Stem Cell 24, 995-1005.e6 (2019).
2. Scientists recreate blood-brain barrier defect outside the body. ScienceDaily https://www.sciencedaily.com/releases/2019/06/190606133837.htm.
3. Ribecco-Lutkiewicz, M. et al. A novel human induced pluripotent stem cell blood-brain barrier model: Applicability to study antibody-triggered receptor-mediated transcytosis. Sci. Rep. 8, 1–17 (2018).
4. Helms, H. C. et al. In vitro models of the blood–brain barrier: An overview of commonly used brain endothelial cell culture models and guidelines for their use. J. Cereb. Blood Flow Metab. 36, 862–890 (2016).
5. Orphanet: Allan Herndon Dudley syndrome. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Expert=59.
6. Daneman, R. & Prat, A. The Blood–Brain Barrier. Cold Spring Harb. Perspect. Biol. 7, (2015).
7. Hypoxia-enhanced Blood-Brain Barrier Chip recapitulates human barrier function and shuttling of drugs and antibodies | Nature Communications. https://www.nature.com/articles/s41467-019-10588-0.
About PHCbi
The “bi” part of our new brand PHCbi is not only a shortened form of the word “biomedical” but also represents both our strength and philosophy as an abbreviation of “biomedical innovation.”
Since the launch of our first Pharmaceutical Refrigerator model in 1966, we have taken advantage of this technology to create exceptional medical and laboratory products and services with a high degree of quality and reliability. We have worked to meet the expectations of customers in the medical and life science fields under both the Sanyo and Panasonic brands. See more detail from "About PHCbi". Find PHCbi's customer case study in the world.